Ontario's 2nd wave of COVID-19 forecast to peak in October

Fresh projections suggest that Ontario's second wave of COVID-19 will peak in mid- to late October and will likely send enough patients to intensive care that hospitals will need to scale back non-emergency surgeries.
The forecasts come from the COVID-19 Modelling Collaborative, a joint effort of scientists and physicians from the University of Toronto, University Health Network and Sunnybrook Hospital.
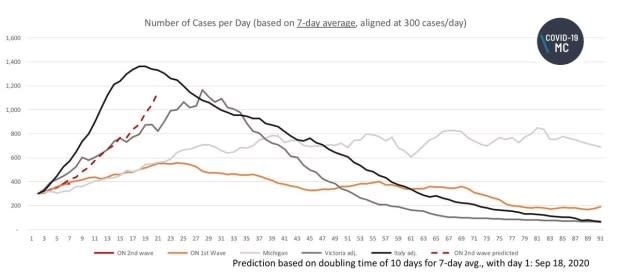
Based on how quickly Ontario's infection rate has been rising in recent weeks, the model projects the province is on track to exceed 1,000 new cases per day by the middle of October, unless stricter public health measures slow the accelerating spread.
The average number of new cases reported daily in Ontario is currently running four times higher than what it was at the end of August. Premier Doug Ford's government has since shrunk limits on the size of private gatherings, reduced opening hours for bars and ordered strip clubs to close.
On Monday, Ontario reported an additional 700 cases of COVID-19, the most on a single day since the outbreak began in late January. The figure surpasses the previous high of 640 from April 24.
On Sunday, Ontario's Ministry of Health reported 112 patients in hospital with a confirmed case of COVID-19, nearly triple the number of two weeks ago. The research team says the impact of the second wave on Ontario's hospitals will depend on the demographics of who gets infected in the coming weeks.
"We are at this critical moment right now where we see case numbers increase and we don't quite know yet where it's going," said Beate Sander, a scientist at the University Health Network and Canada Research Chair in economics of infectious diseases.
"Right now, we have predominantly younger, healthy people (contracting COVID-19 in Ontario)," Sander said in an interview with CBC News. "But what we've seen in other jurisdictions is that it really spills over into other population groups."
The team of researchers has run four scenarios for how Ontario's second wave could play out from here.
The best-case scenario would mimic Ontario's first wave in March and April, when case numbers increased rapidly but were then reined in by a lockdown.
Two moderate scenarios would resemble how a second wave hit jurisdictions comparable to Ontario: the Australian state of Victoria (home to Melbourne, a city of 5 million), and the U.S. state of Michigan.

None of those three scenarios shows COVID-19 patients filling Ontario's hospital wards or ICUs beyond their capacity. That happens only in the modellers' worst-case scenario: a second wave as severe as the first wave that hit Italy when the pandemic began.
However, in all but the best-case scenario, the researchers foresee ICU demand that exceeds the capacity required for patients undergoing scheduled surgeries.
"The really high-risk cancer surgeries, for instance, won't be able to go ahead if the ICUs are overwhelmed with people who are showing up in the emergency department dying of COVID-19 associated pneumonia and respiratory failure," said Dr. Kali Barrett, a critical care physician at the University Health Network and part of the modelling research team.
The researchers stress that their modelling scenarios are simply forecasts. They use data on the proportion of people who have have ended up in hospital and ICUs while positive for the coronavirus, and project those onto Ontario's current trend in new cases.
The shifting demographics of who's getting infected with COVID-19 as the second wave builds makes it challenging for the researchers to forecast just how many people will need hospital treatment.
"The second wave in Spain and France started in the younger populations, but it is spreading to the elderly and the people who are more at risk of ending up in the intensive care unit or in the hospitals," said Barrett in an interview with CBC News.
"It is just a matter of time until this virus, if it's affecting the young populations, spreads into the elderly population," she said. "We're already starting to see that happening in Ontario."
The latest figures from the province's Ministry of Health show 227 people aged 70 or older with an active confirmed case of COVID-19. That number has increased 34 per cent in the space of a week.
Changes in the eligibility criteria for testing can also muddy the forecast. When testing is widespread and captures larger number of mild cases, the percentage who end up in hospital will be smaller than when testing is restricted to priority groups most likely to have the virus, as it was in Ontario in the spring.
Ontario altered its "anyone can get a test" policy on Friday, so far fewer people without symptoms are now eligible for testing.
WATCH | Infectious disease specialist Isaac Bogoch explains whether targeted restrictions will be enough to keep COVID-19 cases in check:
ICU demand could lengthen surgical backlog
Ontario has around 2,000 intensive care beds, and the province plans to add 139 in October. The province's ICU beds are typically two-thirds occupied by patients whose cases have nothing to do with COVID-19, whether it's a heart attack, car accident, or another critical illness.
Since ICUs can't actually function at 100 per cent occupancy full time, the researchers calculate that Ontario has around 475 beds available for non-emergency surgery patients and COVID patients. When scheduled surgeries are running at full pace, those patients take up all but 100 of those beds.
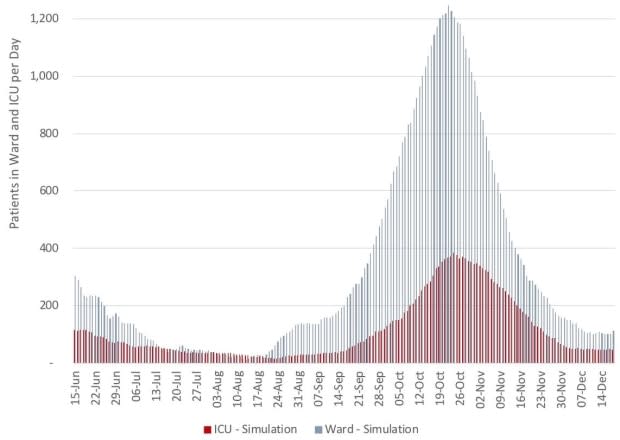
Their conclusion: if more than 100 people with COVID-19 need ICU care, they'd be competing for space with scheduled surgery cases.
"Then we would have to make decisions in terms of who to treat," said Sander. "Do we admit COVID patients or do we do (non-emergency) surgery?"
The projections suggest if Ontario's second wave follows what happened in the Australian state of Victoria — a sharp spike in new infections that drops off quickly after a strict lockdown — some 350 to 400 people will need an ICU bed at peak demand in late October.
If the second wave in this province plays out as Michigan's did — a rise in new infections that levels off but doesn't slow down for a long time — the forecast is for more than 200 patients with COVID-19 in the ICUs from late October onwards.
Figures published Sunday by the Ministry of Health show 28 ICU patients with a confirmed case of COVID-19.
In Ontario's first wave, the number of COVID-19 patients in ICU peaked at 264, while the number of people in hospital at one time peaked at 1,043. Non-emergency surgeries were postponed across the province.
If the majority of Ontario's second wave infections come among younger healthier people — as has been happening through September — hospitalization rates are expected be lower than in the spring.
The modellers say ICU occupancy numbers will be of more critical concern than total hospitalization numbers because Ontario's hospital system can far more easily free up general ward beds than it can make space in intensive care.
That's less about the available beds and ventilators, and more about the having enough doctors and nurses capable of the specialized care that ICU patients need.
"You can't just train people overnight to do this type of thing," said Sander. "You can buy a lot of beds and you can buy a lot of ventilators, but you can't get these highly qualified staff on the ground within a very short period of time."
Barrett agrees that human resources are the key limiting factor, and is concerned about how the second wave could hit hospital staff and their families.
"The majority of people working in hospitals are in their 30s, 40s and 50s, so many of them have children who go to school," she said. "If there is a massive outbreak amongst the younger population and school children, that's a whole sector of our health workforce that won't be able to come to work."
Still have questions about COVID-19? These CBC News stories will help.
Is another lockdown coming in Ontario? What do we know about the Ford government's fall plan?
CBC Queen's Park reporter Mike Crawley obtained a draft copy of the plan
What's the latest on where I should get tested?
It's confusing, but here's an explainer complete with a flow chart
What's the most recent guidance on mask use?
Reporter Lauren Pelley took a look at what the experts are advising
What should I do about my COVID bubble?
With cases going up, even small gatherings are getting riskier
Who is getting COVID-19?
CBC News crunched the data from across Canada to get the clearest picture possible

 Yahoo Movies
Yahoo Movies 
