Inside the Heated Scientific Debate to Redefine Who Is Dead

It was March 10, 2022—day one of a virtual forum held over Zoom to re-write the Uniform Determination of Death Act (UDDA), a draft law that for four decades has been the basis for defining who is alive and who is dead in the United States. Many of those assembled were legal professionals who are members of the Uniform Law Commission (ULC), a quasi-governmental entity whose origins go back 125 years. It’s a crowded meeting of five dozen guests from both the legal and medical realms. Each one was eager to share their own perspective on an issue that at first glance may seem fairly cut-and-dried—until one really starts to dig deep into the legal and medical nuances behind trying to define death itself.
The ULC is the perfect forum for this kind of debate. Pandemonium can arise for laws that left up to states, each different state choosing to abide by its own wildly different set of rules.. When each state—and therefore the U.S. as a whole—would benefit from uniformity, the ULC drafts bills that are then presented to each legislature for adoption. Normally, that means wrestling with relatively mundane issues like child custody or trucking regulations.
That day, the ULC was taking on something more existential. Unfortunately, even matters of life and death are prone to Zoom hiccups. Dr. Malcolm Shaner, a neurologist at University of California Los Angeles, was running into some difficulties while trying to address the group.
“You appear to be muted,” Arizona Court of Appeals judge Samuel Thumma, the chair of the meeting, said with a touch of wry amusement creeping into his voice. His stately image was reinforced by the wall of thick legal books at his back. “Oh, there we go.”
Shaner, wearing a suit and tie that’s completely at odds with the tropical rainforest Zoom background behind him, launched into a monologue about brain stems, reflexes, and their connection to consciousness. Despite the thick medical jargon, many in the digital windows nodded along.
Over the course of several hours, Thumma kept things moving, calling on individual speakers as they raised their hands via digital emoji. In the chat, heated yet respectful debates spilled over each other.
Dr. Doyen Nguyen, a professor of moral theology and bioethics at Atlanta’s Pontifex University, who is also a physician specializing in diagnostic hematology (the study of blood and its disorders), duked it out with Thaddeus Pope, an expert on medical law and clinical ethics at Mitchell Hamline School of Law in Saint Paul, Minnesota. Pope co-authored a January 2020 journal article in Annals of Internal Medicine that first proposed remaking the UDDA.
“Thad: We are dealing with human beings,” Nguyen wrote in the chat. “This is not the place nor the time to impose uniformity for uniformity sake.”
“Doyen: Really? This is the UNIFORM law commission, discussing the UNIFORM determination of death act,” Pope replied.
When drafting legislation, vocabulary counts for everything. Opposing viewpoints were passionately aired over seemingly minute details. Within this group, there were two sides: One believes that death is best described as permanent, and the other believes death is irreversible.
The distinction is subtle, but critical. Fans of the latter definition argue that describing death as “permanent” doesn’t go far enough—death is only permanent if no medical action is taken, but irreversible means that nothing can be done.
A North Dakota doctor by the name of Christopher DeCock, who opted for the bridge of the original Starship Enterprise as his background, used another fantasy tale to make his fandom of Team Irreversible known.
“This isn’t Princess Bride, where you’re mostly dead,” he says, paraphrasing Billy Crystal’s comedic relief healer Miracle Max from the 1987 classic. “Either you’re dead or you’re not dead.”
The debate over when death begins goes back more than half a century. Prior to that, death was rather straightforward: Life ended when the heart and lungs ceased to function. But in 1959, two French physicians, Pierre Mollaret and Maurice Goulon, documented for the first time a phenomenon they observed in two dozen patients who were connected to ventilators.
Unlike someone in a vegetative state, these patients couldn’t breathe on their own, nor did they respond to stimuli, even reflexively. Nor did they show any other signs of life typical of previous patients who lacked consciousness—they did not sleep, for instance. Their brains showed no electrical activity, ruling out any chance of any kind of consciousness. This went further.
Mollaret and Goulon coined a new term for this condition: coma dépassé, or beyond a coma. The bodies lived, but the patients themselves did not.
A few years later, in 1963, a Belgian surgeon named Guy Alexander harvested organs from the body of a patient whose condition was the same as those observed by the French doctors. Since the patient’s organs were still being fed oxygen, they would be in better shape when they were transplanted into living patients. The donor’s brain wasn’t functioning and the donor was in coma dépassé, so what was the problem? Around the world, great numbers of organ transplants followed, including, in 1967, the first successful transfer of a human heart from one body to another.
Families and Physicians Debate the True Meaning of Brain Death
But there was a problem. At the time, death was still defined as the loss of a pulse. By that legal and medical definition, all of those organ donors were still alive.
In 1968, faced with this brave new world of organ transplantation, a small team convened at Harvard University to sort out a modern legal definition of death. Together, the group tried to answer two questions: When has a human brain irreversibly ceased to function? And if the brain has ceased to function forever but the heart continues to pump, is that person dead?
Or, read another way: What is a life?
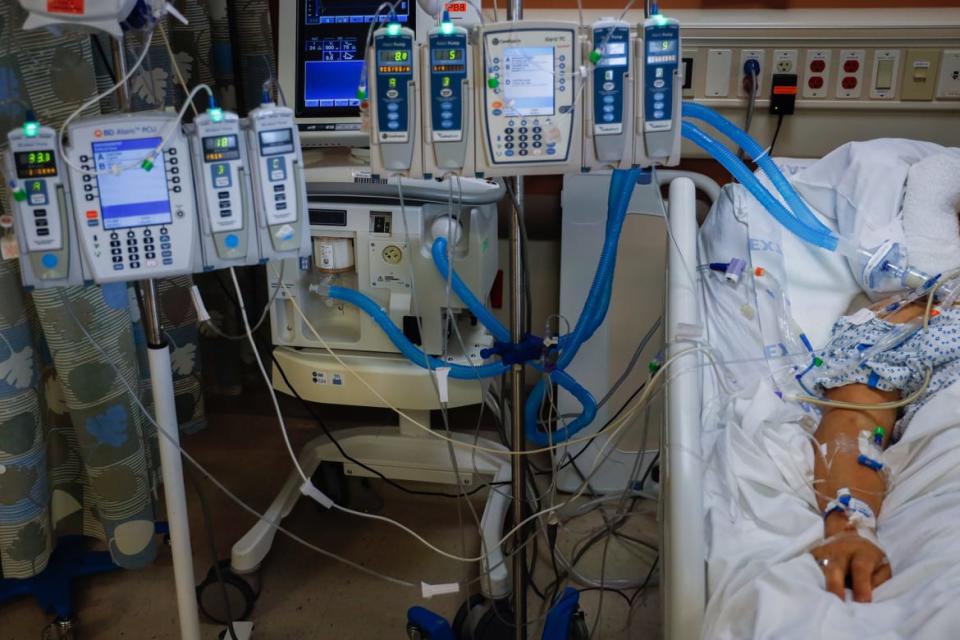
A COVID-19 patient, in a medically induced coma, is connected to life-sustaining devices providing blood pressure medication, antibiotics, sedation, feeding and assistance breathing at Mount Sinai South Nassau Hospital in Oceanside, New York on April 14, 2020.
The landmark Harvard paper laid out some basic criteria for determining when a brain is non-operative. But the authors concluded that this state of “irreversible coma” did not need a legal definition. Whenever lawsuits came up, they said, the courts should simply bow to expert medical opinion. In other words, these new problems in medical ethics would have to be judged case by case.
Alex Capron, a law expert in health policy and medical ethics currently at the University of Southern California, was among the first legal scholars to point out the flaws in this approach. In 1970, Kansas became the first state to enact a clumsily written law recognizing that a still-functioning body could belong to a person who was now legally dead. Other states began following with their own individually written laws. Without a universal standard, Capron argued, death in the United States could become a legal and ethical hodgepodge, with different criteria in different states. That means someone could be alive in New York and dead in New Mexico. The country needed clear, consistent criteria—lest the courts be flooded with lawsuits from anguished family members whose loved ones lay in a legal gray zone between heaven and Earth.
In 1980, Capron was appointed to head up a presidential commission to examine the issue. Representatives from the American Bar Association, the American Academy of Neurology, and the American Medical Association, gathered in Chicago, ultimately concluded there should be two ways to determine death: either when the heart and lungs have stopped working, or when the brain has stopped working.

Alexander Capron at medical ethics conference.
With this guidance in place, ULC commissioners gathered on the Hawaiian island of Kuaui the next year to formally draft a model law governing death—the UDDA. It was a fitting locale: Local legend holds that the island’s Waimea Canyon is home to the souls of the recently dead.
The core of the UDDA consists of just a single paragraph, which defines a dead person as:
An individual who has sustained either (1) irreversible cessation of circulatory and respiratory functions, or (2) irreversible cessation of all functions of the entire brain, including the brain stem... A determination of death must be made in accordance with accepted medical standards.
— The Uniform Determination of Death Act
Those 42 words were the product of almost a decade of work from both doctors and lawyers. Thirty-six states soon adopted the law’s exact language. The rest made only minor revisions. Essentially, the commissioners had formalized brain death, as it became colloquially known. No longer was the line between life and death a simple divide between a beating and a still heart; as the following decades would prove, the line had become remarkably perforated.
In the Zoom call’s chat, Robert Truog, the director of Harvard’s Center for Bioethics and a practicing clinician in pediatric intensive care, had a bone to pick: He wanted to know if the others believed that “whole brain death”—where both the brain stem and the cerebrum are no longer functioning—equated to biological death.
He pointed to the case of a 4-year-old boy who was kept on life support for 20 years. Over the years, he underwent a stunted form of puberty, despite a subsequent autopsy showing his brain had long since calcified. To Truog, this was not a curious but isolated item from the medical archives. Rather, it’s the case that best makes a point he has spent a career hammering home: Human beings do not need a brain to live.
Truog, who holds a philosophy degree from Brown University, has spent much of his career pondering what it means to be alive. While he was working on his internship at the University of Colorado in the early 1980s, the UDDA was unveiled to the world. He was perturbed by what he saw as contradictions in the act’s definition of death.
“It did strike me that there was something odd,” he told The Daily Beast. “We can use medical testing to decide when your kidneys aren’t working, when your lungs aren’t working, when your heart’s not working. And then we use science to think about how to address that.”
But, Truog said, the question of when someone has died is more a metaphysical one than it is a scientific one.
“The question of death is a hugely multifaceted issue that really strikes to the core of the human condition,” he said. “And to think that we could simplify our understanding of death into an algorithm of medical tests struck me, I think, immediately as, ‘There’s something fishy going on here.’”
As his career progressed, Truog became an outspoken critic of brain death as both a medical and legal concept. In 2012, he co-authored a book called Death, Dying and Organ Transplantation: Reconstructing Medical Ethics at the End of Life, laying out a case for doing away with it and suggesting a new paradigm for ethical organ harvesting.
In the book, Truog argues that, had it not been for the advent of vital organ transplantation, brain death as a concept likely would never have been invented. In his view, the idea of brain death was just a convenient way for doctors to avoid contravening their Hippocratic oath, “First, do no harm.”
What if Brain Death Could Be Reversed?
Transplant surgeons abide by what is known as the dead donor rule: They cannot remove vital organs such as hearts and lungs unless the donor is dead. (Non-vital organs, like kidneys, may be removed if the donor is alive, so long as the donor gives proper consent). To remove vital organs from a living patient would be murder.
The problem, as Truog saw it, was that brain-dead patients didn’t meet the criteria for being dead. Yes, their brains had suffered tremendous damage, but so had people in persistent vegetative states, and they were considered alive. Yes, those patients were alive only because of the machines they were hooked up to—but so were kidney patients on dialysis.
And how could the brain be dead if the hormonal system was still functioning? The 4-year-old boy had gone through puberty. Other cases have seen fetuses gestate in brain-dead mothers. Both those processes rely on hormones. The pituitary gland and hippocampus, the body’s hormonal regulating centers, are located in the brain.
“I know Bob Truog and I respect Bob Truog a lot. I think he’s a thought leader,” Sam Shemie, a pediatric critical care doctor at the Montreal Children’s Hospital who has written extensively on brain death, told The Daily Beast. But, “the arguments that are put forward against brain death are quite repetitive and tiring.”
He adds, “When we're talking about death, we're no longer talking about death of all the cells of the body, all the organs of the body, we're talking about a medical-legal definition of death that is based on the presence or complete absence of brain function… The medical and legal definition of death that allows hospitals to work is an understanding of when things can be reversed, and when they cannot. That needs to be scientifically based.”
The gray zone surrounding brain death was perhaps most publicly debated in the case of Jahi McMath, a California teenager whose family fought against a brain death determination after she developed a severe bleed while undergoing surgery for tonsillitis in 2013. The family’s efforts to keep their daughter on a ventilator went so far that they ended up moving to New Jersey, the only state where religious objections can be a reason to keep a person deemed brain dead on life support indefinitely.
Scientists Explain Near-Death Experiences
For a small but vocal group of physicians, these cases aren’t just outliers. At least one of the Zoom call’s participants had called for a moratorium on harvesting organs from the brain-dead, arguing that it’s impossible to be truly certain that brain function has been lost forever. Instead, physicians should disclose the ambiguity to families while seeking consent for organ donation.

Nailah Winkfield, mother of Jahi McMath, sits with her husband, Martin Winkfield, left, while attending a court hearing to discuss the treatment of 13-year-old daughter Jahi McMath in Oakland, Calif., on Monday, Dec. 23, 2013.
Pope noted that for every case that becomes widely known, many others remain obscure. It’s impossible to say just how frequent lawsuits involving the UDDA and its variants have become. And that’s to say nothing of the personal pain that opaque rules on brain death can cause. For every headline-grabbing tale, there are many others that play out quietly in hospital ICUs and hallways where grieving kin are told that a mother or father, daughter or son, lying just feet away with their chest still rising and falling, is not actually alive. Families must reconcile what their eyes are seeing with what the medical and legal realms have deemed a fact.
But exactly how that consideration is determined remains frustratingly ill defined. Under the current wording of the UDDA, brain death must be determined by the “best practices” of the medical community—wording so vague that there can be different requirements for calling someone dead not just between states, but between different hospitals, sometimes in the same city.
The issue isn’t isolated to the U.S.. In 2020, physicians from more than 15 countries joined to co-author an article in the Journal of the American Medical Association. Calling themselves “the World Brain Death Project,” they pointed out that a universal way to pinpoint who was dead was nonexistent. Only around 40 percent of countries had a protocol to determine brain death. Of those, almost all were unique, with massive discrepancies in procedure. Some countries didn’t require checking body temperature. Some didn’t require doctors to make sure patients’ bodies didn’t contain drugs that could mimic brain death. The clinical tests themselves were scattershot—around 10 percent didn’t require an apnea test, in which a ventilator is shut off to see if rising carbon dioxide levels in the blood kickstart autonomous breathing, before declaring someone brain dead.
Physicians and lawmakers around the world couldn’t even agree on what brain death is. In the U.S., the definition requires the entire brain to lose function while other countries define brain death as failure of the brain stem only.
This fractured, hyper-nationalized conception of death could only lead to confusion, the World Brain Death Project claimed. A patient could be considered alive in the U.S. and dead in the United Kingdom.
Dozens of organizations representing medical experts from around the world, including the World Federation of Neurology, endorsed the initiative.
Even as the experts on the Zoom call were ping-ponging ideas on what the new law will require, some on the call were worried about what would happen once that consensus is reached. The new law’s wording isn’t expected to be agreed on before 2023. After that, it will have to go to 50 state legislatures (as well as the bodies governing areas like Puerto Rico and Washington D.C.) for approval. Although many states passed the original UDDA with little fanfare in the years following 1981, politics since then has gotten much uglier.
“It seems absolutely obvious to me that in South Dakota, Oklahoma, Ohio, a number of states, this is going to be a big problem,” Pope said at the meeting. “We’re literally legislating what states of life are worth protecting, which is very, very similar to the abortion debate.”
On June 24, the Supreme Court reversed Roe v. Wade, the pivotal ruling that for almost half a century enshrined abortion as a constitutional right. As millions of people expressed their anguish, several states immediately moved to outlaw the procedure, with several others likely to take action to severely restrict, or even ban, abortions in the near future.
There is worrying precedent.
In 1981, shortly after the wording of the original UDDA was approved, Capron appeared on ABC’s Nightline. Host Ted Koppel interviewed Capron, and then pivoted to an opposing view from a physician named Mildred F. Jefferson, the first Black woman to ever graduate from Harvard Medical School. Jefferson was one of the most ardent anti-abortion advocates in the country. (She was perhaps best known for convincing Ronald Reagan to become pro-life).
As the segment wrapped up, B-roll footage from the Western Massachusetts Hospital played. Nurses attended to prone, motionless patients.
In voiceover, a reporter declared that 25 patients in the hospital “have no brain waves and, by Massachusetts state law, they are legally dead. But even they continue to breathe on their own, without the use of machines.”
Today, 41 years later, Capron is still incensed at the error.
“People in persistent vegetative states are not the people who are going to be determined to be dead,” he said. Those people may have suffered serious injuries, but since they breathed without the help of machines, they were not brain-dead. Brain death and persistent vegetative states are often confused by the public. Capron fears the mixup could be used to push a narrative—under today’s even more partisan climate, death could once again become a victim of political culture wars.
He pointed to the case of McMath.
“Once that became an issue, she was, of course, embraced by the Right to Life Community,” he told The Daily Beast. “And they were saying basically the same thing that this woman had said on Nightline, which is that you are taking people who are not dead, and for the wrong reasons, calling them dead so that you can take their organs or whatever.”
Perhaps the clearest case of the political fighting that can break out over end-of-life issues came during the years-long saga of Terri Schivao, the Florida woman who suffered massive brain trauma resulting in the diagnosis of a persistent vegetative state in 1990. When Schiavo’s husband decided to remove her feeding tube, saying his wife wouldn’t have wanted to continue living in her condition, her parents sued to have it kept in. The matter escalated to the point that Congress and then-President George W. Bush intervened, passing special legislation to send the matter to a federal court after a judge ruled the tube should be removed.

Terri Schiavo and her mother taken at Terri's hospital bed in 2003 in Gulfport, Florida.
Though Schivao was able to breathe on her own, and therefore wasn’t brain-dead, the argument over who gets to determine what level of life is worth preserving became a media and political firestorm that dominated cable news for weeks.
Over the past decade, Truog has come to an uneasy peace with brain death. He’s spent too much time in an ICU, declared too many patients brain-dead, overseen too many organ procurements, spoken to too many colleagues to believe his views will ever become mainstream.
Instead of seeing death as a biological state, he now sees it as a social construct. He still believes that doctors are engaging in a form of justified homicide if they remove organs from a brain-dead patient, even with full consent. But he acknowledges that convincing his peers and the general public of his stance “will never fly.”
“It is not unreasonable,” he said, “to say that when a person will never wake up again, will never breathe on their own again… that means they can be treated as dead, and for legal purposes could be considered dead.”
Get the Daily Beast's biggest scoops and scandals delivered right to your inbox. Sign up now.
Stay informed and gain unlimited access to the Daily Beast's unmatched reporting. Subscribe now.

 Yahoo Movies
Yahoo Movies 
