‘Don’t talk about Covid’: major parties accused of virus complacency during election campaign

The federal election campaign is “clearly a case of Covid Fight Club,” Prof Stuart Turville says. “Don’t talk about it.”
Turville, a virologist at the University of New South Wales, wonders when Australia’s continuous Covid-19 deaths and slowing booster shot rates “will become an issue of discussion within our government”.
Almost 7,900 Covid deaths have occurred in Australia since the pandemic began, with at least 66 of those on Tuesday alone, and 53 more on Wednesday. More than 1,000 deaths were reported in the past month.
Meanwhile otherwise healthy, triple-dosed people are reporting coronavirus symptoms significant enough to require bedrest for days, as hospitals and the broader health system buckles, not only because of the virus infecting staff but also because of years of under-resourcing and under-funding. And many Australians are still wondering if they will eventually need a fourth dose of a Covid vaccine, or if existing vaccines will be tweaked to better respond to new variants.
Related: Emergency overload: how Covid exposed Australia’s straining hospital system
The current vaccines are extremely effective at achieving their primary task: preventing people from developing severe disease and ending up in hospital. But Covid infection rates in Australia are rising, leaving immunocompromised and other vulnerable people who are less protected by the vaccines particularly worried.
Rates of people getting their vaccine booster doses are slowing: about 19.7m Australians aged 16 and over are double-dosed, compared with about 13.6m who have had three or more doses.
Neither major party has announced policies or new funding for vaccinations or the long-term impacts of Covid ahead of the election.
“Time will tell us how complacency at many levels will play out,” Turville says.
“What will happen if we don’t get our third or fourth dose? Will we see the death rate per day creep up from 40, to 60, to 80 before we start to talk about this again?
“We need to ensure those who have been working on the response to this virus keep at it. The best way to do that is for the government and also industry to continue to fund the response.”
‘The Band-Aid is being ripped off’
Experts say that funding must include better tracking of Covid-19 infection rates and deaths within Australia, as international comparisons have become less meaningful given vast differences in how countries test and report cases.
It used to be easier to track the virus and compare data. For a long time, because of restrictions, few people were infected in Australia, allowing almost every case to be studied. There were no vaccines, so researchers could determine how the immune system responded to the virus alone. There were far fewer variants, making it clearer what any one strain of the virus was doing.
Turville says now “the Band-Aid is being ripped off”.
“The immunity in the community is a real mix,” he says. “It’s a hybrid of prior infection then vaccination, or vaccination then infection, or a booster then infection. It’s interesting at many levels, but also complex.”

This mix of variables also makes it harder to study how long protection against the virus lasts.
“Modelling a decaying [immune] response now involves several starting points,” Turville says.
“Was it your booster, or your last Covid-19 infection?”
Small changes in the virus were tolerated by the available vaccines, which responded well to the Delta and Alpha variants. But then Omicron came along.
“The viral entry pathway changed and in doing so the virus crawled up the respiratory tract,” Turville says.
“Many people are infected with Omicron following their booster dose. They can readily transmit it as well. The fact is, we still don’t know how this immunity will track over time, and more importantly, what variant we will meet in the future.”
Prof Sharon Lewin, an infectious diseases physician and director of the Doherty Institute, says what this will all mean for Australia’s vaccination program is being considered by the Australian Technical Advisory Group on Immunisation (Atagi), which advises the government.
“We do know from large studies, primarily from Israel, that immunity against Omicron gradually wanes after the third dose, meaning your protection against infection reduces,” Lewin says.
“But your protection against hospitalisation is quite well maintained after your third dose, which is really the most important thing. Israel has shown in older populations 60 and above, a fourth dose further reduces risk of hospitalisation, including from Omicron.”
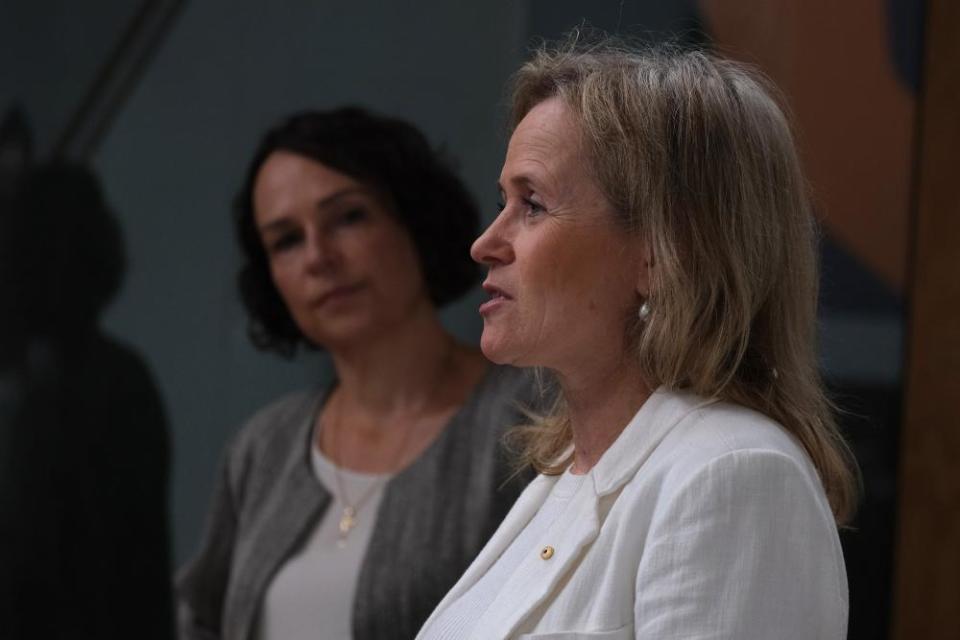
Atagi recommends certain groups receive a fourth dose to maximise their protection against severe illness. That includes adults aged 65 and older, Aboriginal and Torres Strait Islander people over the age of 50, aged care and disability care residents, and anyone aged 16 and older who is severely immunocompromised.
“At the moment, the benefit of protection against hospitalisation from a fourth dose hasn’t been shown for the general population,” Lewin says. “That may change as we get more data, and Atagi are actively monitoring the situation.”
In the meantime, Prof Julie Leask, from the University of Sydney’s Institute for Infectious Diseases, says two-dose coverage in Australia “has definitely hit a high ceiling” at 95.6% for those aged 16 and above.
Booster coverage is now at 70%, and primary schooler double-dose vaccination coverage is at 53%. Leask believes without ongoing vaccine campaigns and attention from governments, the vaccination rates in these groups will only “slowly crawl upwards”.
“We need to increase our booster coverage, particularly for people at highest risk of severe disease,” Leask says. “This remains urgent particularly as we head into winter.
Related: Why are Australia’s Covid case rates still so high and how can we prevent more deaths?
“We also need high flu vaccination coverage. This is always an issue, but this time there is more immune naivety in the population from two years without much flu.”
Leask says it is frustrating to see a lack of political urgency around these issues.
“Unfortunately, public health seems to have dropped off the radar all together in the lead-up to the election,” she says.
“The new government should urgently review our vaccination situation and plan a national campaign to both remind and persuade people to be up to date with their vaccinations. More broadly, we need to know what the major parties plan to do about a pandemic review, and public health workforce.”
It remains unclear why so many eligible people aren’t getting their third booster dose, Leask says.
“Australia needs timely and routine deep-dives on why people don’t vaccinate, so we can target the strategies,” she said.
“Second guessing people leads to inefficiencies, because governments sometimes assumes they know and can miss the mark. Once the disease comes, it’s too late. This is the most challenging thing about promoting vaccine uptake.”

 Yahoo Movies
Yahoo Movies 